Mechanism of neonatal diabetes discovered
Published : 18 Dec 2018, 03:47
Updated : 18 Dec 2018, 12:05
Researchers at the University of Helsinki have described mechanisms linking chronic cellular stress to poor development of the insulin-producing cells.
Insulin is secreted from the beta cells located in the pancreas and it is crucial for the maintenance of normal blood sugar levels, said the University of Helsinki in a press release referring to a study.
Deficiency of insulin leads to diabetes, characterised by elevated blood sugar. Diabetes most commonly presents in childhood as Type 1 diabetes and in adults as Type 2 diabetes.
Sometimes diabetes is diagnosed already in very small babies, during the first six months of life. In these cases, mutations in the gene encoding insulin are often found.
These mutations are only found in one copy of the gene; that means that half of the insulin produced is normal, which should be enough to secure normal blood sugar.
However, this is not the case: insulin secretion stops totally after a few months. It is believed that this is caused by a toxic effect of the mutant insulin inside the cell, but the exact mechanisms are understood poorly.
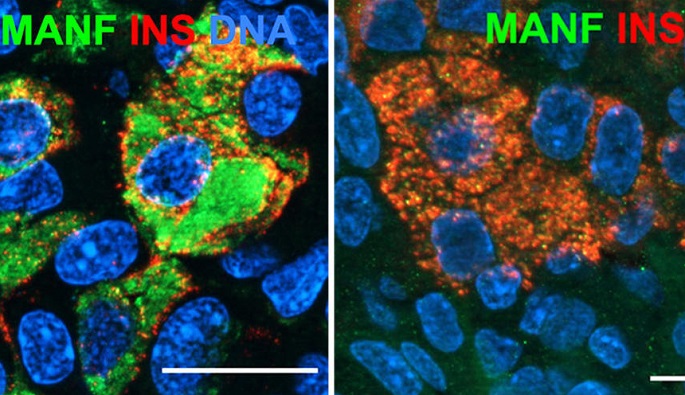
Mutant insulin is known to cause a chronic stress reaction in the beta cell, and it has been thought that this leads to the death of the cell. It is important to understand the detailed consequences of beta-cell stress, because this may help in developing drugs for preventing both rare and common forms of diabetes.
“We now had the chance to test this with real patient-derived cells,” said Professor Timo Otonkoski of the University of Helsinki.
Researchers created a human disease model using stem cells from people carrying insulin gene mutations; then they corrected cells using a gene editing technique called CRISPR.
The mutant and corrected stem cells were then induced to turn into insulin-secreting beta cells and the researchers followed the function of the cells after transplanting them in mice.
“The main finding of the study was that these cells do not die from the chronic stress, but their growth and development is disturbed. These effects are mediated through processes that could potentially be targeted by drugs,” said Diego Balboa.
“In this study, we describe mechanisms linking chronic cellular stress to the poor development of the insulin-producing cells. A strongly reduced number of beta-cells will cause diabetes immediately, but even a milder defect will increase the risk of diabetes later in life. Understanding the molecular mechanisms of these processes may help in devising ways to preserve the mass and function of beta cells,” said Otonkoski.